Pulmonary Rehab Case Study
Mr. S.C. arrived at North End Rehabilitation and Healthcare Center after an acute care stay at Beverly Hospital for respiratory failure, pneumonia and sepsis due to the COVID 19 virus.
- 12/10/2021: Required intubation due to an inability to wean from the ventilator.
- 12/23/2021: Required a tracheotomy due to his deteriorating respiratory status and remained on the ventilator to support his respiratory state.
- Mr. S.C. required placement of a feeding tube to maintain adequate nutrition.
- During his acute hospitalization, Mr. S.C had become encephalopathic and was both physically and mentally debilitated and deconditioned requiring total care.
After several weeks in the hospital, Mr. S.C.’s mental state began to improve, his encephalopathy cleared, and he returned to his baseline cognition. However, he now required aggressive rehabilitative therapy to return to his previous physical state. Mr. S.C was eventually weaned from the ventilator and successfully transferred to North End Rehabilitation and Healthcare Center to continue his rehabilitation, where he was admitted into our Pulmonary Rehabilitation Program.
Admission Assessment
- Required maximum assistance with all personal hygiene: bathing, dressing, shaving, toileting, bed mobility, ambulation and transfers.
- Decreased balance and deconditioning
- High fall risk
- Limited participation secondary to generalized weakness and deconditioning.
Nursing Interventions
- Maximum assistance with meals, personal hygiene, bathing and dressing, and tracheotomy care and management.
- Tracheotomy: Care and management provided by a dedicated 24H respiratory therapy team and supported by our pulmonology services, resulting is successful decannulation.
- Maintaining proper nutrition via feeding tube care and management.
- Monitor Labs and Vital Signs
- Medication management
Rehabilitation Interventions
- Initial Assessment: Maximum assistance with transfers in and out of bed, in and out of a chair and with ambulation up to 10 feet.
- Evaluated by PT, OT and ST: treatment modalities implemented including focus on regaining his swallowing strength, with a goal of successfully returning to oral eating.
- His feeding tube was successfully removed, and he was able to eat without signs or symptoms of aspiration.
- PT and OT worked collaboratively on strengthening and conditioning, balance and ambulation and he successfully regained the ability to ambulate and complete activities of daily living independently.
- Maintain and educate patient on safety awareness with transfers and ambulation
Interdisciplinary Team Approach
- Mr. S.C. benefited extensively from skilled physical, occupational, speech, and nursing therapies in a multidisciplinary approach to achieve the most optimal clinical and psychological outcome. Both his strength and memory improved substantially throughout the course of his rehabilitation.
Discharge Assessment
- Actively engaged with the IDT and eagerly participated in care team meetings and therapy.
- Personal Goal: After aggressive efforts of the entire interdisciplinary team, Mr. S.C. achieved his personal goal, which was to regain his strength and mobility. He was able to return home with home care services within 30 days of his admission. Frequent check-ins were completed with Mr. S.C post discharge, and he continues to do well. He has had no further hospitalizations and has remained clinically stable.
“I am so grateful for the care I received here at North End. Because of them, I am going home. The team here is the absolute best!”
Case Study
Admitting Diagnosis: Displaced Intertrochanteric Fracture of the Left Femur
Discharge Location: Home
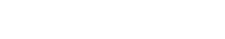
A 91-year-old gentleman who was admitted to The North End Rehabilitation and Healthcare Center from Spaulding Rehabilitation Hospital for skilled nursing and therapy following a left femur fracture. Upon admission, Mr. C. was evaluated by and participated in skilled occupational and physical therapy where he was noted to require stand by assistance with upper body dressing and maximum assistance with lower body dressing. He required moderate assistance for toileting and bathing and contact guard assistance with hygiene and grooming. Additionally, he required minimum assistance with bed mobility, moderate assistance with transfers and contact guard assistance to ambulate 5 feet with a rolling walker. Mr. C. was determined to return home and he consistently participated in therapy. Upon discharge, Mr. C. was able to do 13 steps with contact guard assistance and was able to transfer and ambulate 300 feet with a rolling walker and supervision. He was also able to perform upper body dressing with supervision, lower body dressing with minimum assistance, and was able to perform bed mobility with modified independence. He made great gains toward his therapy goals and was able to return home at an increased level of independence with strong family support and VNA services. Great job, Mr. C.!
10.0 – Complete Independent – No assist, no equipment
9.0 – Modified Independent – No Assist, but equipment or extra time
8.0 – S/u – No physical assist other than set-up; supervision for safety/technique; and/or single cue to initiate
7.0 – Supervision-No physical assist; supervision for safety/technique; and/or single cue to initiate
6.0 – SBA-Pt. performs task with close supervision and or visual/verbal cues for task completion
5.0 – CGA – Contact Guard Assist
4.0 – Min – Occasional assist (25% or less time or effort to complete)
3.0 – Mod – Frequent assist (40-50% of the time or effort involved to complete task
2.0 – Max – Constant assist (75-90% of the time or effort involved to complete task
1.0 – CD – Complete Dependence: No contribution from pt; task done by others or not assessed
Case Study
Admitting Diagnosis: Cerebral Infarction
Discharge Location: Home
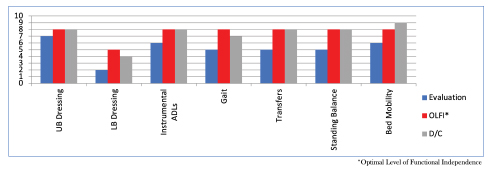
A 76-year-old female who was admitted to the North End Rehabilitation and Healthcare Center from Mass General Hospital for skilled nursing and therapy services to safely return home following a cerebral infarction. Upon admission, Ms. K. was evaluated by and participated in skilled occupational, physical and speech therapy where she was found to require maximum assistance for lower body dressing, minimum assistance for bed mobility and contact guard assistance for transfers, gait, toileting, upper body dressing, and hygiene. Additionally, she was put on a mechanical soft texture diet to reduce risk of aspiration and required moderate cueing for problem solving. She was determined to return home and worked hard with the therapists to return to a more functional level. Upon discharge, Ms. K. was able to transfer and ambulate 350 feet independently, was able to perform all self-care tasks without assistance and was able to be upgraded to a regular diet, showing vast improvement with her safety during swallowing activities. She made great gains toward her therapy goals and was able to return home with home health services. Great work, Ms. K.!
10.0 – Complete Independent – No assist, no equipment
9.0 – Modified Independent – No Assist, but equipment or extra time
8.0 – S/u – No physical assist other than set-up; supervision for safety/technique; and/or single cue to initiate
7.0 – Supervision-No physical assist; supervision for safety/technique; and/or single cue to initiate
6.0 – SBA-Pt. performs task with close supervision and or visual/verbal cues for task completion
5.0 – CGA – Contact Guard Assist
4.0 – Min – Occasional assist (25% or less time or effort to complete)
3.0 – Mod – Frequent assist (40-50% of the time or effort involved to complete task
2.0 – Max – Constant assist (75-90% of the time or effort involved to complete task
1.0 – CD – Complete Dependence: No contribution from pt; task done by others or not assessed